All you need to know about the low FODMAP diet
by Harry • 8 minutes read
Last updated: 29 Aug, 2022
Most often recommended to those with Irritable Bowel Syndrome (IBS) and/or small intestinal bacterial overgrowth (SIBO) - the low FODMAP diet focuses on lowering the intake of fermentable carbohydrates.
IBS is the most common gastrointestinal disorder, affecting between 25 and 45 million people in the US. For many people with IBS, food is one of the biggest triggers for symptoms like bloating and stomach pain. (1) This is where the low FODMAP diet comes in - promoting an eating style that reduces the stress on the digestive system.
What are FODMAPs?
“FODMAP” stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols.
These are the scientific terms given to the group of carbohydrates that tend to cause digestive discomfort for some people.
FODMAPs are typically short chain carbohydrates (sugars) that the small intestine absorbs poorly - this is where discomfort begins.
These foods are osmotically active, which means they encourage water into your digestive system. Also, as they are non-digestible, they are fermented by our gut bacteria which in turn increases short-chain fatty acid production and gas in our digestive tract. (1) (2)
In fact, about 60% of people with IBS have reported that these carbohydrates may either cause or worsen their symptoms. (1)
Various foods contain FODMAPs, so steering clear of them entirely will be quite difficult, but limiting your intake is certainly possible. To help, here's a breakdown of what foods are high in FODMAPs:
Oligosaccharides: nuts, wheat, legumes, rye, garlic, artichokes, and onion.
Disaccharides: milk, yoghurt, soft cheese, ice cream, whipped cream and the like.
Monosaccharides: fruits such as apples, mango and pears - plus sweeteners such as agave nectar, high fructose corn syrup and honey.
Polyols: apples, pears, cauliflower, mushrooms, and low calorie sweeteners, such as those in sugar-free gum and mints
The digestive discomfort produced by the foods above, comes in many forms, but these are a few of the most common symptoms:
Cramping
Diarrhoea
Constipation
Stomach bloating
Gas and flatulence
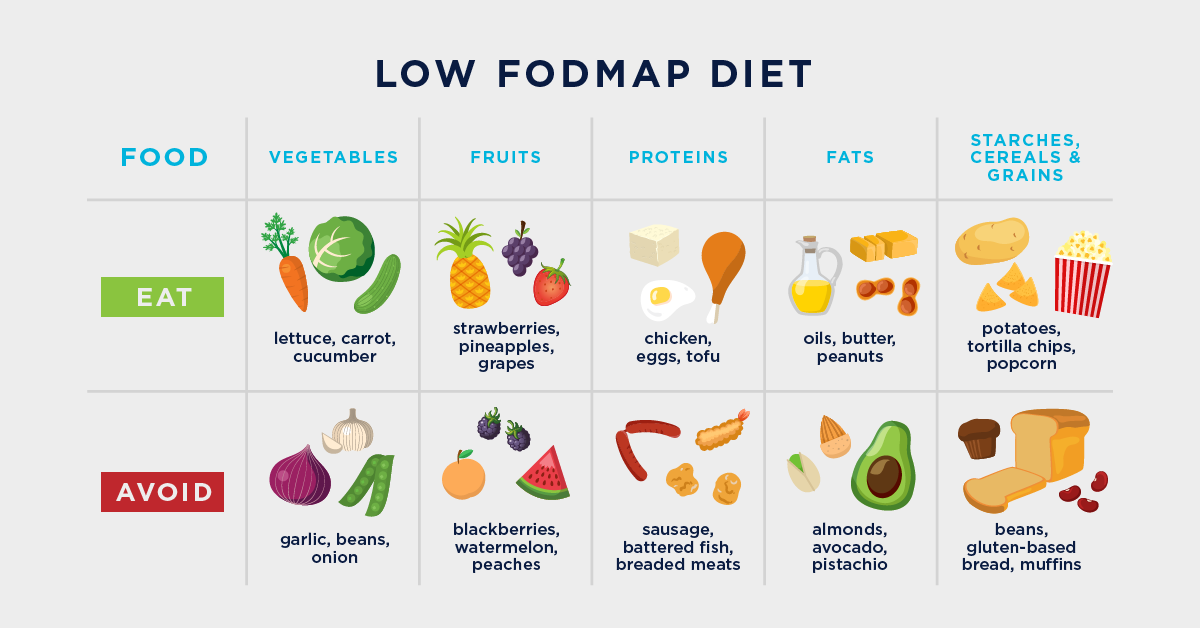
What foods can you eat on a low FODMAP diet?
Most people will consume between 15-30 grams of FODMAP carbohydrates per day. A low FODMAP diet aims to limit that daily intake to roughly 2.5-3 grams - which corresponds to 0.5 grams per sitting (when you follow the recommended frequent but small meal structure). (1)
This may seem like a huge reduction, but there are plenty of foods and food groups that are naturally low in FODMAPs that would be recommended in this diet: (3) (4)
Vegetables: bean sprouts, bell peppers, radishes, carrots, celery, eggplant, kale, tomatoes, spinach, cucumber, pumpkin, and zucchini
Fruit: blueberries, raspberries, pineapple, honeydew melon, cantaloupe, kiwi, limes, guava, starfruit, grapes, and strawberries
Whole grains and starches: white and brown rice, lentils, corn, oats, quinoa, cassava, and potatoes
Proteins: beef, chicken, eggs, fish, lamb, pork, prawns, tempeh, and tofu
Seeds and Nuts: almonds (no more than 10 per sitting), macadamia nuts, peanuts, pecans, pine nuts, and walnuts
Dairy: lactose-free milk, Greek yoghourt, and Parmesan, Colby, cheddar, and mozzarella cheeses
Oils: coconut and olive oils
Condiments: cumin, saffron, cinnamon, paprika, coriander, cardamom, soy sauce, fish sauce, ginger, mustard, pepper, salt, white rice vinegar, and wasabi powder
Drinks: peppermint tea and water. Coffee and other teas are also low in FODMAPs but they tend to cause discomfort for those with IBS, so they aren't encouraged in most low FODMAP diets.
Who should try a low FODMAP diet?
The most common purpose of adopting a low FODMAP diet is to alleviate the digestive problems experienced by those with IBS, but this is not the only reason to try the diet.
A research group first discovered that it could help manage the symptoms of IBS in 2005. (5) Since then, over 30 studies have been conducted, testing the effects of limiting FODMAPs upon those with IBS. With one in 10 adults suffering from the digestive disorder, IBS, it's no surprise so much research has been done into the subject.
These studies have repeatedly found that the diet can reduce the effects of IBS, with one systematic review and meta-analysis of 22 studies, finding that a low FODMAP can improve:
Overall digestive symptoms
Abdominal pain and bloating
Quality of life
Gas
Diarrhoea and constipation
We must note that most of the diets administered in these studies were developed by registered dietitians, and if you are seeking dietary help, please speak to a professional to ensure the safest and best results.
More importantly, the same studies were largely conducted with only adult subjects, so there is very little evidence supporting the benefits of a low FODMAP diet for children. (6)
Some speculate that a low FODMAP diet may also have other benefits - namely aiding weight loss due to the restriction of carbohydrates, which are often high in sugar and calories.
Others also suggest that the diet may help reduce symptoms of other conditions, such as diverticulitis and exercise-induced digestive issues - but the evidence for this is rather limited. (7) (8)
How to use a FODMAP diet for IBS relief
There are three simple and clear steps that are recommended for those looking to reduce FODMAP foods in their diets to relieve IBS symptoms.
Warning: We always recommend consulting a medical professional or licensed dietitian before beginning a new diet.
Step 1: FODMAP elimination
Objective: Identify the foods which are high in FODMAPs in your diet.
Take a look at what high FODMAP foods are and switch out those in your diet for low FODMAP foods.
Some may begin to feel better after just a few days, but it can take up to 2 weeks to begin relieving symptoms of IBS. Bear in mind that in this phase, you should avoid cheat days - the closer you keep to the diet restrictions, the better you will feel and the faster you will feel it.
The time spent in this phase usually varies between 2-6 weeks but this will depend on the personal medical advice you receive.
Step 2: FODMAP reintroduction
Objective: Work out which FODMAP foods affect you most.
This phase requires paying great attention to how each new food affects your symptoms. Once your body has adjusted to the lack of FODMAPs, you should start slowly reintroducing high-FODMAP foods into your diet and observe how they affect your digestive system.
If a certain food causes no change or discomfort, then you can include it in your regular diet going forward. If it does trigger symptoms, then you can cut it out of your diet.
Note: each FODMAP subgroup should be reintroduced separately, with at least a few days between each reintroduction. This allows you to more easily observe which foods have which effects on your body.
This phase usually takes between 6-8 weeks.
Step 3: FODMAP integration
Objective: establish a FODMAP diet that works for you.
Once you have established which foods affect you most, you can focus on reintroducing those that were more tolerable. Eventually, the goal is to create a diet that contains the FODMAP foods that suit you best and eliminate those that cause discomfort.
It’s important to note that exclusively following a low FODMAP diet long-term, will not be healthy or practical. The purpose of a low FODMAP diet is to temporarily relieve discomfort but you cannot sustain it permanently. You should use a low FODMAP diet to discover what foods suit you best and build a more comfortable diet heading forward.
Other things you should know
A low FODMAP diet is not a no-FODMAP diet
The low-FODMAP diet is not a FODMAP elimination diet. It is designed to limit your intake of FODMAPs to reduce digestive discomfort, not to eradicate them completely.
A low FODMAP diet is not a long term diet
It is not recommended to undertake a low FODMAP diet for more than 8 weeks as a whole. You should follow the 3 simple steps that are often suggested for those beginning a low FODMAP, which should ensure a healthy transition to the change in nutrients.
Can a low FODMAP diet be nutritionally balanced?
Of course! You can and should get everything you need in a low FODMAP diet, but it is important to note that, like any diet, there is always a risk of nutritional deficiencies.
For a low FODMAP diet, you should keep an eye on both fibre and calcium intakes in particular. (9) (10)
We aim to always give appropriate credit to our reference sources and image authors. Contact us if you think a credit may be incorrect or you're an author and would like to request removal.






